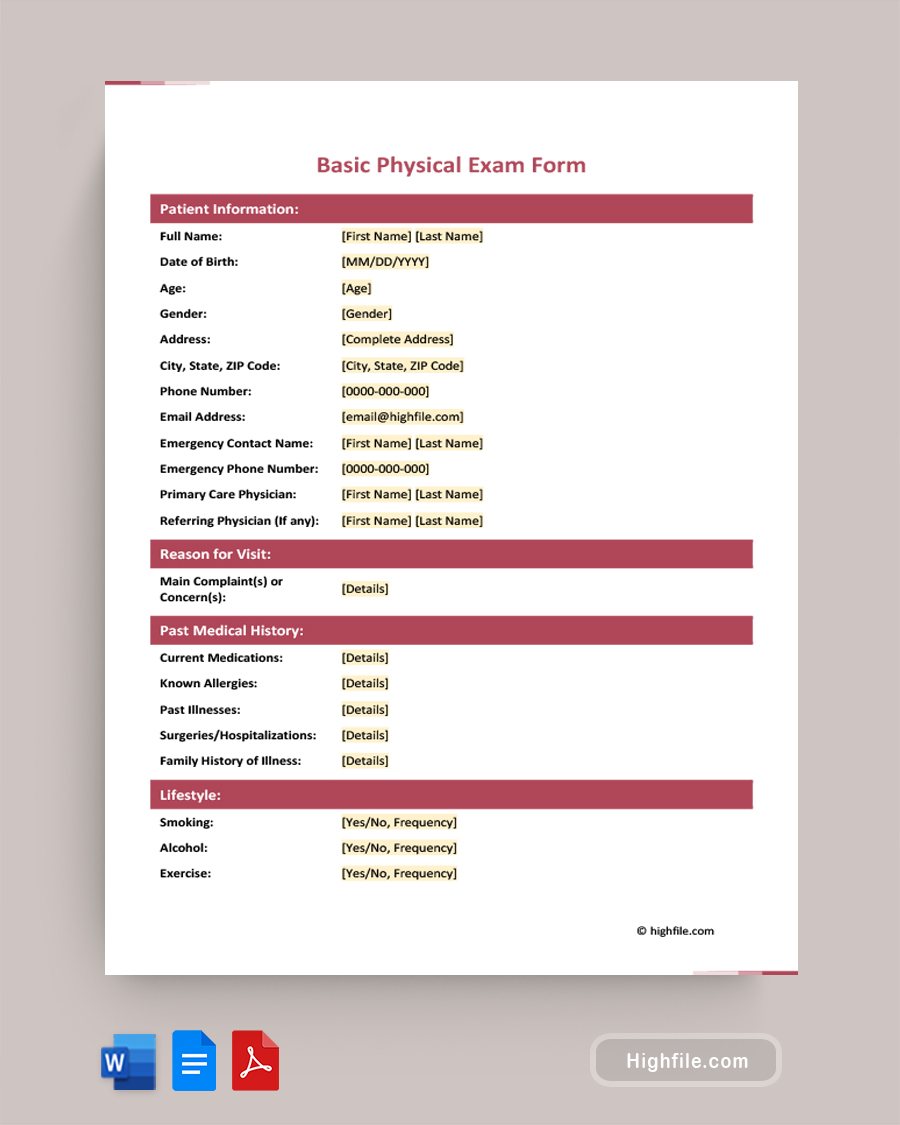
A Basic Physical Exam Form is a comprehensive document healthcare providers use to record and conduct routine physical examinations. This form gathers essential, standard patient information. For example, it usually includes medical history, lifestyle habits, and any results from physical examinations or lab tests. It is helpful to assess the patient’s overall health, identify potential health risks, and formulate appropriate treatment plans or follow-up care. We’ve provided the basic physical exam form template in Word, PDF, and Google Docs for your convenience.
About Basic Physical Exam Form
A Basic Physical Exam Form is an integral document healthcare professionals use to record the results of thorough physical evaluations and address patients’ health concerns. Here are the components typically found in a professional Basic Physical Exam Form:
- Form Title: The title “Basic Physical Exam Form” at the top prevents confusion and helps with recordkeeping.
- Patient Information: The healthcare professional gathers basic identification details, emergency contact information, the primary care physician’s name, and, if relevant, a referring physician’s information
- Reason for Visit: Patients should specify the reason for seeking medical attention or scheduling the physical examination. That data is recorded here.
- Past Medical History:
- Current Medications: List any medications they take, including prescription and over-the-counter drugs.Known Allergies: Record any known allergies to medications or other substances.Past Illnesses: Note any significant past illnesses or medical conditions.Surgeries/Hospitalizations: An area for adding in prior surgical procedures or hospitalizations when relevant
- Family History of Illness: Having information about the patient’s family history of medical conditions or illnesses can help assess risk and treat known issues.
- Lifestyle: This section has information on lifestyle habits such as smoking, alcohol intake, exercise routines, dietary preferences, and other relevant factors.
- Review of Systems Chart:
- System: Lists various body systems, such as respiratory, cardiovascular, gastrointestinal, etc.
- Details: Provides space for medical staff to describe any findings or issues related to each system.
- Physical Examination Chart:
- System: Enumerates different body systems that should be examined during the physical evaluation.
- Findings: Records the findings and observations for each system during a physical examination.
- Lab Results Chart: This section is only sometimes necessary but should be included in a template as it is needed frequently. It can be left blank when not required.
- Test Name: Lists the names of specific lab tests conducted.Results: Records the test results for each corresponding test.
- Normal Range: Provides the normal reference range for each test result.
- Assessment and Plan: Summarize the healthcare provider’s evaluation of the patient’s health here. Next, outline the treatment plan, or follow-up care needed.
- Physician Information: List the healthcare provider’s name, contact details, and any relevant credentials.
- Consent Statement, Signature, and Date Lines: Includes a consent statement for the patient to review. They authorize the examination and any additional tests or treatments by signing here.
FAQs
If you don’t know the answer to a field in the medical history section, be honest and provide the most accurate information available. If unsure about details, you can leave the field blank or inform the healthcare provider during the physical examination. They can assist you in filling out the form correctly or advise you on obtaining previous medical information.
You should include over-the-counter medications in the ‘Past Medical History’ section under ‘Current Medications.’ Unfortunately, these medications can interact with prescription drugs or have potential implications for your health. Your healthcare providers must comprehensively understand all the medications and supplements you are taking to prescribe appropriate and safe treatments.
If your physician hasn’t provided a follow-up plan in the ‘Assessment and Plan’ section, you should inquire directly during the physical examination. If you forget or don’t notice immediately, call, email, or schedule a consultation to discuss the issue. It is essential to communicate with your healthcare provider to ensure appropriate care and management of your health, but follow-up isn’t always necessary if you are in good health.