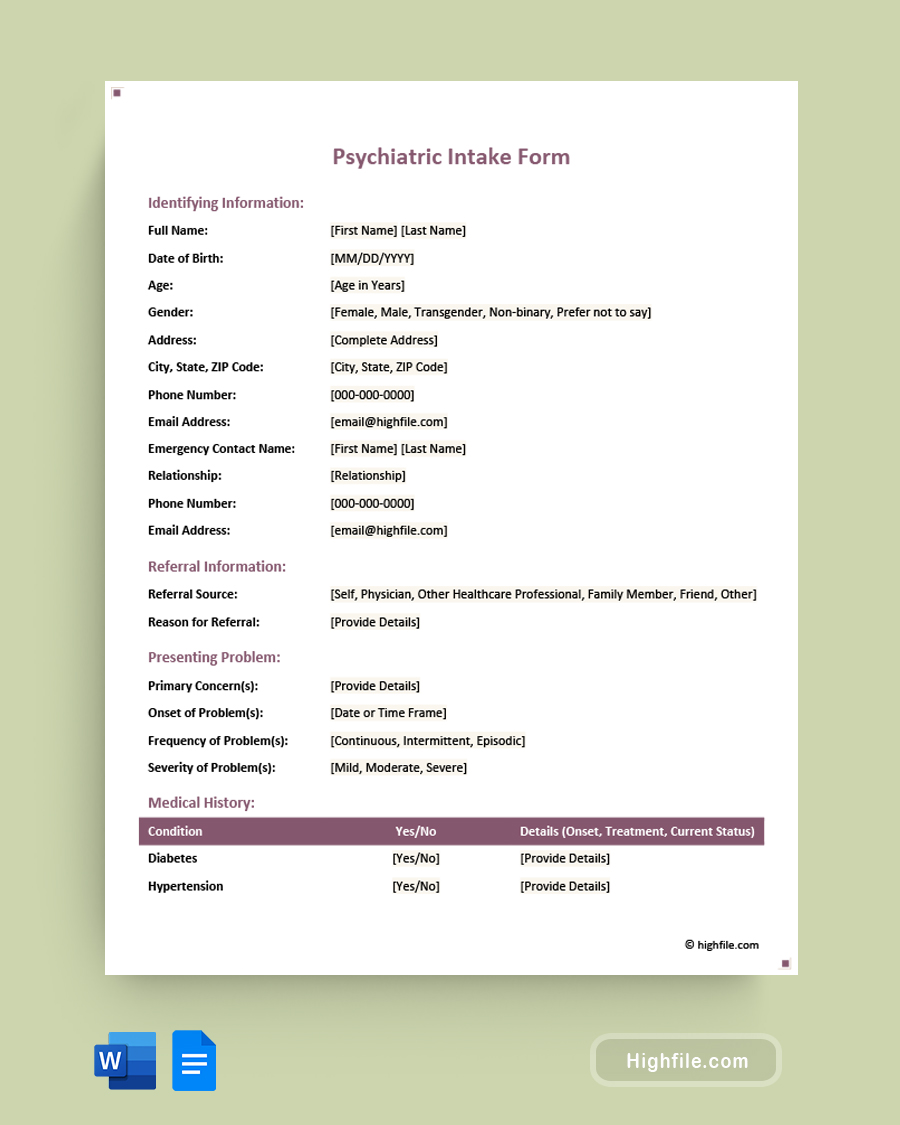
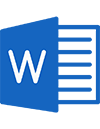
Contents of the Template:
- Identifying Information: Vital patient details, contact, and emergency contact info.
- Referral Information: Who referred the patient and why.
- Presenting Problem: Description of the main concern(s) prompting the evaluation.
- Medical History: Any medical conditions, current medications, and allergies.
- Psychiatric History: Past mental health diagnoses, hospitalizations, and family history.
- Substance Use History: Consumption details of various substances.
- Social History: Marital, familial, educational, and legal details.
- Mental Status Examination: Observations about patient’s current state.
- Risk Assessment: Evaluating the potential for harm to oneself or others.
- Diagnostic Impressions: Preliminary and differential diagnoses.
- Treatment Plan: Setting goals, recommending interventions, and planning follow-ups.
Why Use This Template:
- Efficiency: Streamlines the intake process, ensuring no critical detail is missed.
- Consistency: Guarantees a uniform data collection approach for every patient.
- Clarity: Clear sections and categorization facilitate easy and quick reference.
- Flexibility: Available in multiple formats to cater to various user preferences.
Ideal For:
- Mental Health Clinics: Perfect for standardizing the intake process across a practice.
- Private Practitioners: Helps solo practitioners maintain an organized patient database.
- Hospitals: Ensures a systematic approach to admitting psychiatric patients.
- Research Settings: Collects consistent baseline data for mental health studies.
- Educational Institutes: Useful for training students about the psychiatric evaluation process.