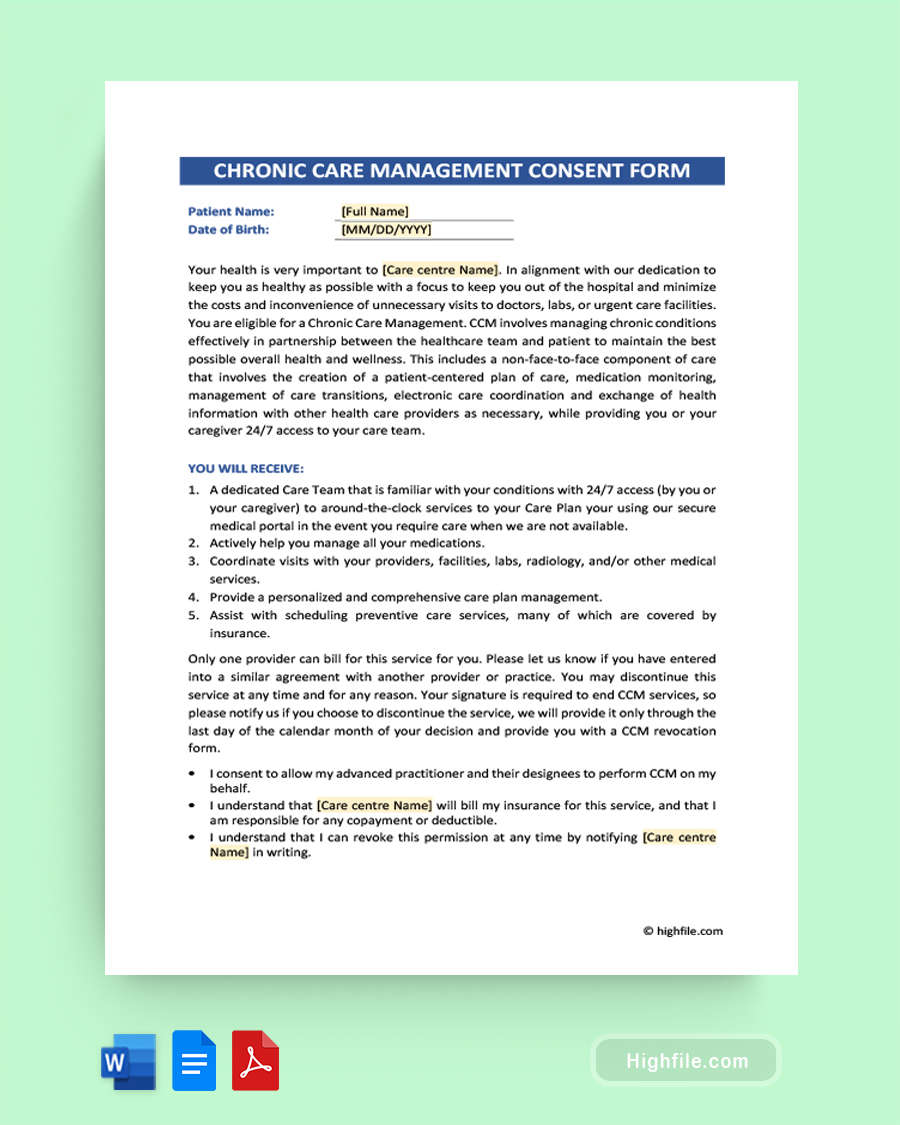
Medical practitioners need Chronic Care Management Consent Forms to ensure that their patients understand the variety and scope of the services provided and are aware of any associated risks. This integral document allows the practitioner to obtain patient consent for various treatments and services and to document their agreement with the treatment and services provided. The form also serves as a way for the practitioner to obtain authorization from the patient for any additional care or treatment that may be necessary. By having this form in place, medical practitioners can ensure that their patients clearly understand what they are receiving and any potential risks associated with those treatments. We strongly recommend using a Chronic Care Management Consent Form template when creating your documents. They provide a structured format that helps save time and ensure that all the correct data is included.
What Is a Chronic Care Management Consent Form?
A Chronic Care Management (CCM) Consent Form is a document that allows a healthcare provider to offer comprehensive and continuous healthcare services to patients with chronic health conditions. The form outlines the patient’s rights and responsibilities regarding the CCM services and the provider’s commitment to providing these services. It also includes information about the types of services included in the CCM program, any applicable fees, or other related topics. The consent form is a legally binding document that must be signed by both the patient and the healthcare provider for the CCM services to be provided.
Why is the Informed Consent Form Important for Chronic Care Management?
Informed consent forms are important for chronic care management because medical practitioners cannot provide treatment without consent. While consent is almost always a necessity, it is especially vital for ongoing, often long-term treatments like those for chronic conditions, and here is why:
- Respects patient rights
- Protects doctors from litigation
- Legally required
- Part of the medical documentation process
- Serves as a record of both consent and treatment
- Builds trust with the care provider
Essential Elements of Chronic Care Management Consent Form
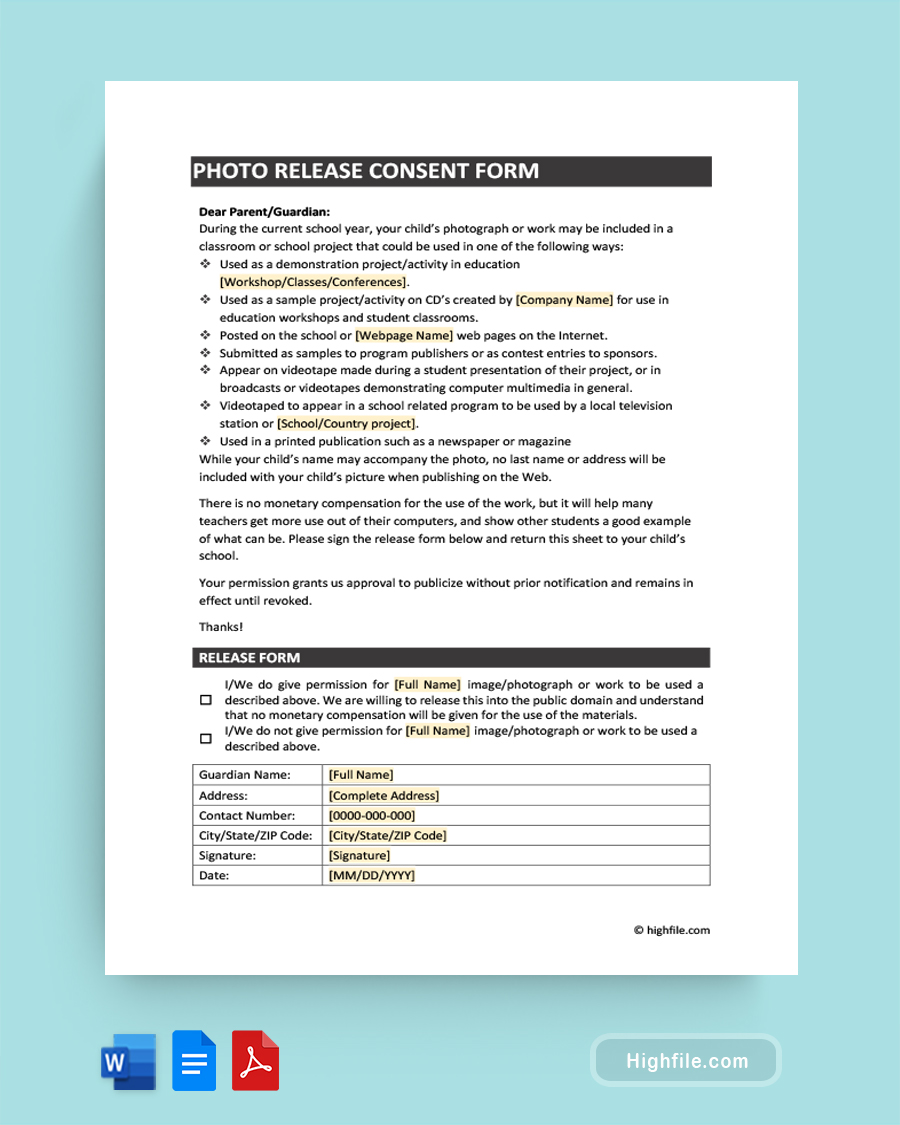
The essential elements of a Chronic Care Management Consent Form include explaining what to expect from treatments, statements of assent, and other vital information. Below we’ve created an outline detailing each aspect of this crucial document and why it needs to be included.
- Business Logo or Name- Including the name or a professional business logo at the top of all your forms is standard practice. It helps with brand cohesiveness and identity.
- Form Title- Titles on official documents should always be large-print, bold lettering that is easy to read and specifies exactly what it contains.
- Client Name and Birthdate- This identifies who is giving the consent.
- Introduction- Introduce the patient to the form, CCM, and your practice.
- Expectation/Options- Here, you should list what the patient will receive and how that will help them, going into specific detail.
- (Optional) Assent Statements- You can include some basic agreements here, such as liability waiver.
- Payment Information- Explain how CCM is billed and any details they need to know.
- Specific Consent Statement- This should state exactly what the patient is consenting to.
- Consent Checkbox- Although redundant, a checkbox next to a simplified consent statement, such as “I agree to participate in CCM treatment,” ensures there is no confusion.
- Signature and Date Lines- The patient and their representative should sign and date at the bottom of the form.
Pro Tip: Customizing the consent form to suit the individual patient is essential. Since there are many options within the umbrella of Chronic Care Management, you may need to address more than one form of treatment within this form. Consider the individual patient’s needs, history, and preferences when creating your custom CCM consent forms.
How to Use a Chronic Care Management Consent Form
Using a chronic care management consent form is relatively simple. Below we’ve listed the steps to make it easier for you.
- Create- Download and fill out a template to create your form. Remember to use simple language and edit and run spelling and grammar checks.
- Explain- Introduce the form and explain its purpose to the patient.
- Deliver- Give the form to the patient and let them read it.
- Review and Answer- Go over the document’s details with the patient. Please encourage them to ask questions and give them answers.
- Obtain Consent- Signing the form is a requirement to provide treatment, so ensure the patient does this.
- Copy and Share- Make a copy and give it to the patient for their records.
- Keep as a Record- Keep the original consent form in your records for as long as the patient works with you, plus 3-7 years for documentation purposes. Ensure this form is also incorporated into the patient’s medical records.
Following these steps will help ensure you have informed consent and proper documentation.
Legal and Ethical Considerations for Chronic Care Management Consent Forms
The use of consent forms is an integral part of chronic care management. These forms provide a legal and ethical framework for treating patients with chronic conditions. Below we will give an overview of the legal and ethical considerations associated with consent forms for chronic care management. We will discuss the importance of informed consent and the need to provide accurate information to and about patients. We will also highlight the need for clear communication between healthcare providers and patients to ensure all parties know the risks associated with chronic care management.
- Informed Consent- Informed consent involves signing consent documents, but anyone can write their name on a form. In order to obtain informed consent, you must give the patient a deeper understanding of the services and treatments you will provide. The patient is not informed without knowledge and comprehension, and their consent may be invalidated.
- Legal Requirements- Local, state, and federal laws all have specific requirements and regulations that you must adhere to when documenting any medical process.
- Patient Rights- A patient’s rights are vital to the medical profession and those seeking treatment. Ensuring they are respected and the patient understands them is a part of your job.
- Respect- Beyond the patient’s bill of rights, it is important to respect individual needs, preferences, and cultural or religious aspects of their needs.
- Privacy- Medical records are kept private because patients have the right to decide who they choose to share information about their bodies with. Moreover, it helps prevent discrimination and even harassment.
- Medicare Records- Medicare requirements are a fundamental part of CCM. You must meet these standards to get paid for your time and work.
- Medical Records- Keeping a history of the patient’s medicines, treatments, and other medical experiences is vital to their future well-being and can help prevent adverse reactions or other significant problems.
- Communication- You must keep an open line of communication with patients to ensure they understand their treatments and to foster trust. Likewise, communicating with medicare, insurers, and other doctors are necessary to do your job efficiently.
Improving Patient Outcomes
Improving patient outcomes is a complex ethical consideration, so we’ve given it a separate category. Aspects such as quality of life and promoting preventative care in Chronic Care Management (CCM) require a multi-faceted approach. The key components of successful and effective CCM are patient education, improved communication between patients, providers, and caregivers, and more coordinated care plans.
Patient consent and education are essential to improving outcomes in CCM. Patients must understand their diagnosis, treatment options, available resources, and disease management strategies. Providers should ensure patients can access reliable and up-to-date information regarding their condition. This can be done through educational materials, web-based self-care tools, and connecting with other patients.
Another critical component of successful CCM is the development of more coordinated care plans, which are patient-centered plans that outline individualized treatment and care coordination. Coordinated care plans should be developed collaboratively between patients and providers to ensure they are evidence-based and aligned with individualized treatment preferences and goals. Patients should also be involved in developing their care plan through an organized disease management approach, which consists of a team effort between patients, providers, family members/caregivers, social workers or case managers/coordinators, dietitians, and other specialists and care providers.
FAQs
CCM is a challenging yet gratifying field to work in. We’ve answered the most frequently asked questions about this topic to help you get the most out of your Chronic Care Management Consent Form. You will find more information about electronic consent, Medicare compliance, and working with patients with low medical literacy, among many other valuable facts.
If a patient refuses to sign the Consent Form for Care Management (CCM), healthcare providers should explain the purpose of the form and the benefits of signing the document. They should also explain the consequences of not signing the consent form, such as being unable to access certain services or treatments. If the patient is still unwilling to sign, healthcare providers should document the conversation in the patient’s medical chart and note that the patient refused to sign. Providers should also be sure to follow up on any concerns the patient may have had about signing the form.
Healthcare providers can ensure that the CCM Consent Form is clear and easy to understand for patients with low health literacy by taking additional steps to clarify the form.
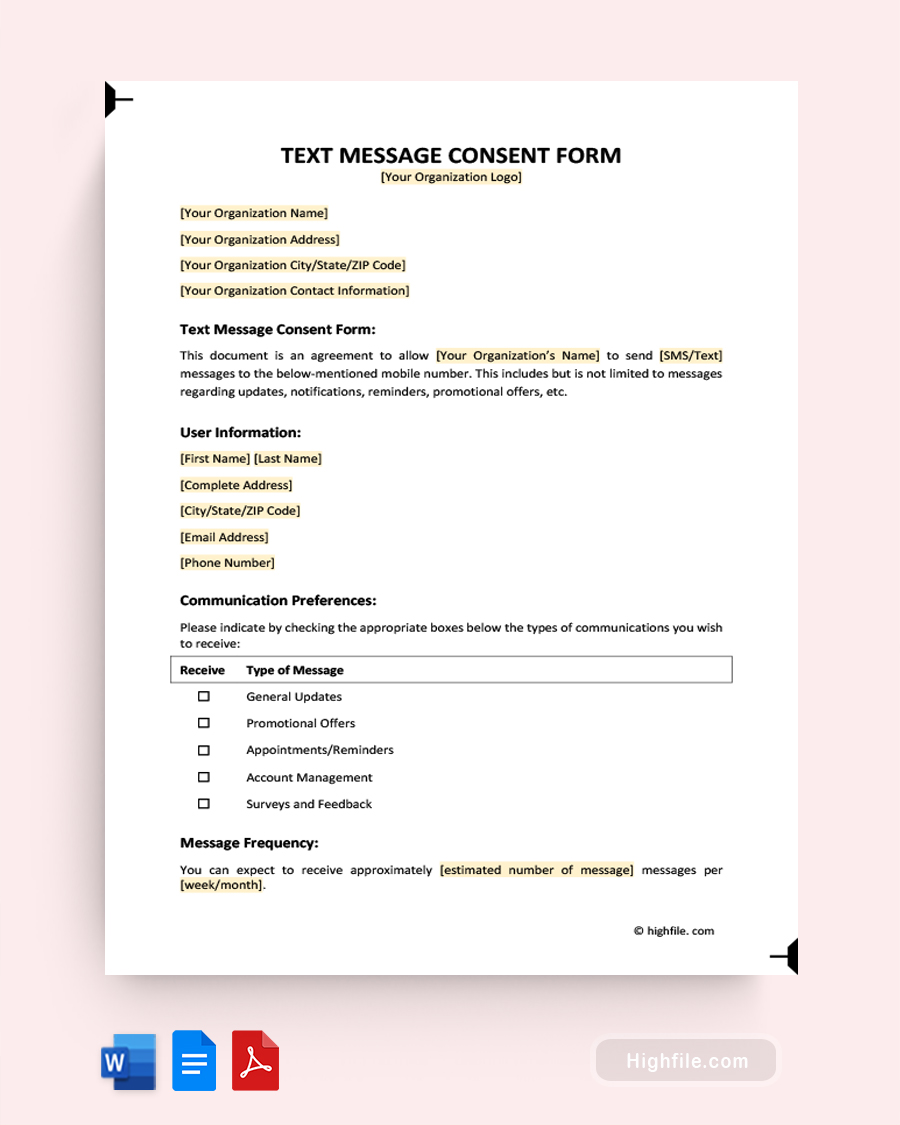
ᐅ Use simple language and avoid medical jargon when communicating the information on the form.
ᐅ Review the document with the patient and provide verbal explanations of the form’s content to help patients better understand what they are consenting to and be prepared to explain it in a different way if necessary.
ᐅ Ensure that the document is presented in a way that is easy to read. Doing this includes providing a large font size and using high-contrast colors.
ᐅ Use simple icons or visuals to explain essential concepts or details. Charts and other imagery are a great way to help people understand how a process works.
ᐅ Encourage questions and be prepared to answer them in simple terms.
Healthcare providers can ensure that their CCM Consent Form complies with Medicare requirements and state laws by taking the following steps.
ᐅ Consult with legal counsel to inquire about applicable laws. Have an attorney read over your form.
ᐅ Carefully review the Centers for Medicare and Medicaid Services (CMS) regulations regarding CCM services.
ᐅ Make any necessary adjustments or additions so the document includes all necessary information required by Medicare and state laws.
ᐅ Keep yourself up to date on the latest changes to Medicare and local or federal laws.
ᐅ Promptly update your CCM consent form when anything changes.
ᐅ Have existing patients sign a copy of the revised form before their next treatment.
ᐅ Always keep your CCM consent forms stored somewhere secure.
If a patient revokes their consent to participate in the CCM program, healthcare providers should respect the patient’s wishes and terminate the CCM program. Healthcare providers should document this in the patient’s medical record and communicate the revocation to all relevant parties, such as other healthcare providers involved in the patient’s care. The healthcare provider should also inform the patient of any potential risks associated with revoking their consent and provide resources for additional information and support if necessary.
It is possible for patients to provide consent for the CCM program electronically. Most CCM programs require the patient to sign an informed consent form before enrolling. Many programs now allow patients to consent electronically via a secure online form. The process is generally simple and takes only a few minutes to complete. Electronic consent forms can be completed on the program’s website or through an app on the patient’s mobile device. By signing the electronic form, patients indicate that they have read and understand the information provided about the program, that they are aware of their rights as a participant, and that they voluntarily consent to proceed.
Healthcare providers can ensure that patients have had the opportunity to ask questions and receive additional information before signing the CCM Consent Form by taking the time to discuss the form with the patient. Providers should explain the terms of the document and its implications in an understandable way. They should also provide additional information about the CCM program and answer any patient questions. Providers should also ensure that the patient understands they have a right to refuse to sign the consent form if they feel uncomfortable with it. Finally, providers should document their conversations with the patient in their records to show the effort was made. These recordings can be reviewed to help steer future discussions in a direction that allows the care provider to clarify or otherwise adjust the focus of the conversation to steer it toward a place of understanding.
Final Thoughts
Informed consent forms are essential to chronic care management, as they help ensure that patients are fully aware of the risks and repercussions associated with their treatment plan. By signing a Cronic Care Management Consent Form, patients acknowledge the potential risks, benefits, and implications of any medical procedure or treatment plan. This allows medical professionals to provide the best possible care for their patients. Informed consent forms also help protect the patient and the medical professional from any potential legal action. By signing a document, the patient agrees to abide by the terms of the treatment plan and releases the medical professional from liability. A professionally designed template can help you create a high-quality, reusable document that is easy to update quickly.