Contraception and women’s rights is a crucial topic that has been in the news often lately. As a result, many doctors see more requests for IUDs and similar long-term pregnancy prevention. When you offer this high-demand service, ensuring all patients sign an IUD Consent Form is vital. Doing this shows that they agree to the procedure and fully understand their patient rights, risks, side effects, benefits, and alternatives. As a healthcare provider, you can use your consent document to help guide the conversation on this critical issue. We recommend using our IUD Consent Form template to help create a high-quality, informative document that is quick and easy to customize for your practice.
What Is an IUD Consent Form?
An IUD Consent Form is a document used to obtain informed consent from a patient before inserting an intrauterine device (IUD). This document outlines the potential risks and benefits of having an IUD inserted and requires the patient to acknowledge that they understand and accept these risks. The form also includes essential information about the procedure, such as what types of anesthesia will be used, what kind of IUD will be inserted, and any other instructions indicating how a patient should prepare before the procedure and what aftercare or additional appointments, checkups and other responsibilities they have afterward. By signing the IUD Consent Form, the patient agrees to proceed with the insertion of the IUD and is giving consent for the placement.
Why Is IUD Consent Form Important?
The IUD consent form is important because it helps to ensure that the patient is fully informed about the risks, side effects, and benefits of using an IUD. The document serves as a legal document that outlines the patient’s consent to use the device. It also helps to protect the patient and the healthcare provider from any potential legal issues.
Historical Fact: The history of the IUD consent form is deeply tied to the rise in informed consent practices. While these clever contraceptives have been around since the early 1900s, health and safety concerns in the 70s and 80s led to a rise in the regulation and development of safer IUDs. Along with better devices, consent forms have become more regulated and comprehensive, containing more information and requiring fully informed consent.
When Is IUD Consent Form Needed?
An IUD (intrauterine device) consent form is typically signed by the patient and their doctor at least twice. First, they sign at the consultation visit to ensure the patient has had ample opportunity to ask questions and request clarifications. Then, prior to the insertion of the device, the clinician and patient sign the form again to ensure the consent is still present. In some cases, they may even sign a third time. If the cervix is too tightly closed at the scheduled time, the patient may need to reschedule for later or earlier in their menstrual cycle, in which case they may need to consent again when the actual insertion occurs.
Essential Elements of IUD Consent Form
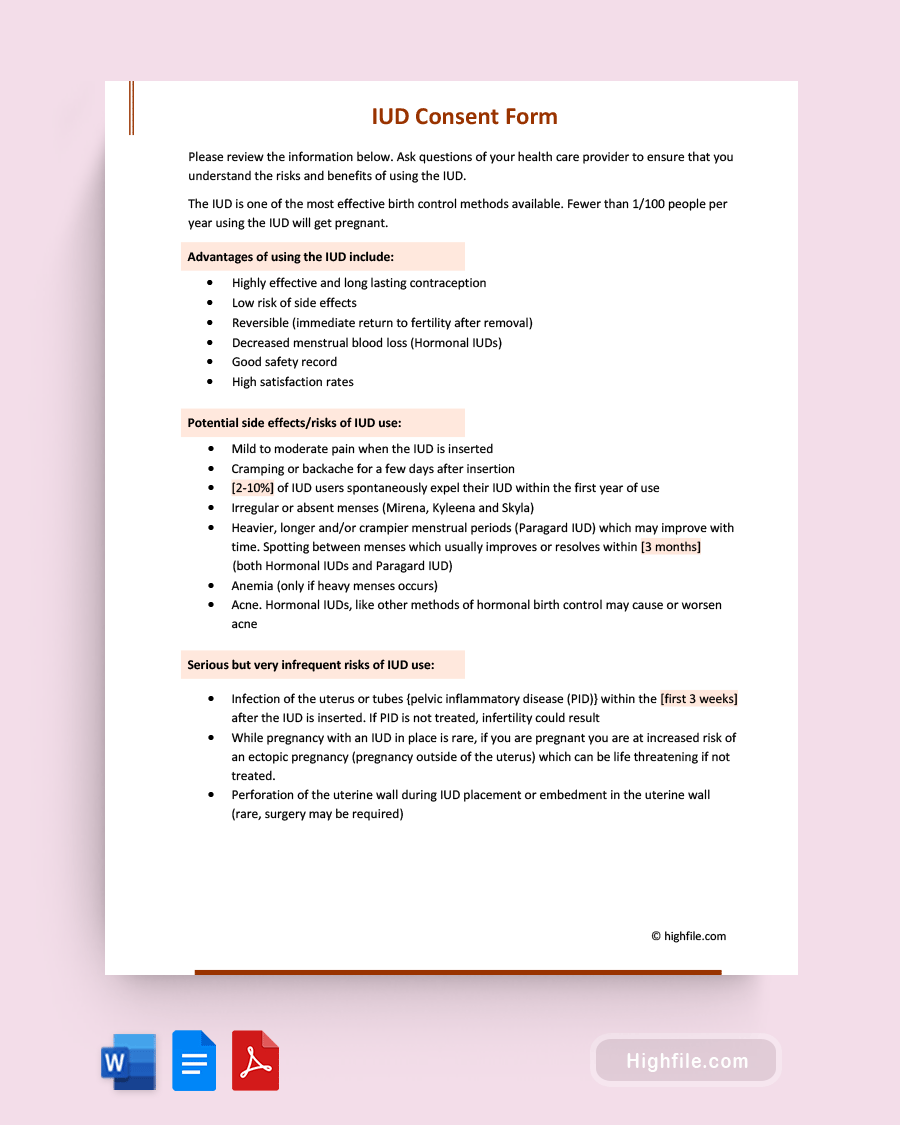
The essential elements of an IUD consent form primarily deal with the side effects, benefits, and risks involved in the procedure. However, you should also provide information about STD prevention, emergency care, the right to have the device removed, efficacy, and more. Below we’ve created an outline to help you better understand the sections of the template and their purpose.
- Form Title- The title should read “Intrauterine Device (IUD) Consent Form” in large bold print.
- Read Statement- This statement asks the patient to read all the information on the sheet carefully.
- Efficacy Statement- Briefly explain that this device is one of the most effective forms of birth control.
- Benefit Statement- List all the benefits of having an IUD
- Side Effects and Risks- List the common side effects and risks here.
- Serious Risks- It’s vital to inform patients of the more serious possible risks, even though these are rare.
- Tertiary Visit Statement- Explain why a second placement visit is sometimes needed when the cervix is too tightly closed.
- Disease Risk- Let the patient know that pregnancy prevention is not the same as disease prevention, and they should still use condoms or other STD preventatives.
- Additional Warnings and Information- This section should include facts about using alternative contraception when the strings cannot be located, when, where, and how to seek emergency services, avoiding the risk of pregnancy before insertion, and the right to removal.
- Understanding Statements- The understanding statements show that patients have had ample time to discuss the relevant information with their provider, know the risks and benefits, have read this form completely, and consent to the IUD placement.
- Patient Consult Signature and Date- This is where the patient signs their consent during the consultation.
- Clinician Consult Signature and Date- By signing after the consultation, the clinician certifies that they believe the patient understands the information and is giving informed consent.
- Patient Placement Signature and Date- Re-signing at the time of placement ensures that the patient has not changed their mind.
- Clinician Placement Signature and Date- A final signature here completes the contract so the doctor can place the IUD.
Pro Tip: It is vital to ensure that your IUD consent form is easy to read and understand. Avoid overcomplicated or industry-specific terminology, be prepared to explain things differently with visual aids if necessary, and choose a font and size that facilitate understanding.
Anesthesia and IUD Insertion
Unfortunately, IUD insertion can be painful, and anesthesia can help to reduce or eliminate the pain or discomfort. You need separate consent for anesthesia when doing IUD insertion. The patient should be informed of anesthesia’s potential risks and benefits before giving consent. The anesthesia provider should be notified of any medications or allergies the patient may have to ensure the safest possible administration of anesthesia.
Discussing Risks, Side Effects, and Alternatives to an IUD
The IUD is a long-term, reversible contraception option that is highly effective and becoming increasingly popular. However, doctors must discuss the risks, side effects, and alternatives to an IUD with their patients before prescribing it. An IUD can cause a variety of potential complications, including device failure. Discussing the other options and shortcomings ensures they can make an informed decision about whether or not the IUD is right for them.
When healthcare providers fail to discuss alternative treatments with their patients, they may face legal consequences. Depending on the situation, a healthcare provider may be held liable for medical malpractice if they fail to provide their patient with information about alternative treatments that could have been beneficial. Sometimes, a patient may sue for damages if they can prove that the healthcare provider’s negligence caused them harm. In addition to potential legal consequences, failing to discuss alternative treatments with patients can also lead to a breakdown in the doctor-patient relationship.
The known risks include perforation of the uterus, heavy bleeding, infection, and ectopic pregnancy. Another issue to consider is that after the procedure, the patient may be at risk of pressure from other pelvic organs. The IUD Consent Form typically includes information on what happens if there is uncomfortable pressure. Patients must understand that they should seek emergency care if they experience any signs of perforation or heavy bleeding, including sharp pelvic pain and fever above 101 degrees Fahrenheit.
IUD Contraindications
IUDs are a popular and highly effective form of birth control, but they are not suitable for everyone. Including a checklist to help prevent those who would not be good IUD candidates from consenting to the procedure without providing complete medical information to you is one of the best ways to avoid serious problems. Common contraindications for IUDs include, but are not limited to, the following:
- Unexplained vaginal bleeding
- Pelvic infection
- History of ectopic pregnancy
- Abnormal development of the uterus
- Active genital or urinary tract infections
- Certain types of cancer
- Allergy to any of the materials used in the IUD
- Recent childbirth or miscarriage
- High risk for STDs or HIV/AIDS
- History of pelvic inflammatory disease
- History of perforation, pelvic abscess, or rupture
- History of ectopic pregnancy “Tubal ligation” or “fallopian tube destruction “History of low progesterone levels
- History of cervical scarring, cervical stenosis, cervical incompetence, or cervical misalignment
FAQs
Below we’ve answered the most frequently asked questions about this procedure and its consent documents. Here you’ll learn more about additional paperwork patients must sign, legal requirements for your document, and other valuable facts.
A patient cannot complete an IUD Consent Form without the assistance of a healthcare provider. This is because the form requires detailed discussion between the patient and provider to ensure that the patient understands the risks and benefits of an IUD. Additionally, the document requires a signature from the patient and provider to ensure that all parties are in agreement regarding the IUD insertion. Without this discussion and signatures, an IUD Consent Form cannot be considered valid.
The IUD consent form template must include specific legal requirements to be valid. These requirements include:
ᐅ A clear explanation of the risks and benefits associated with the IUD procedure.
ᐅ Full disclosure of any potential side effects or complications that could arise from the procedure.
ᐅA statement explaining the patient’s right to withdraw consent at any time. 4. An acknowledgment from the patient that they have read and understand all of the information provided in the consent form, including the risks and benefits associated with the procedure.
ᐅ A statement from the patient acknowledging their consent to the IUD procedure.
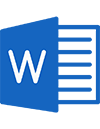
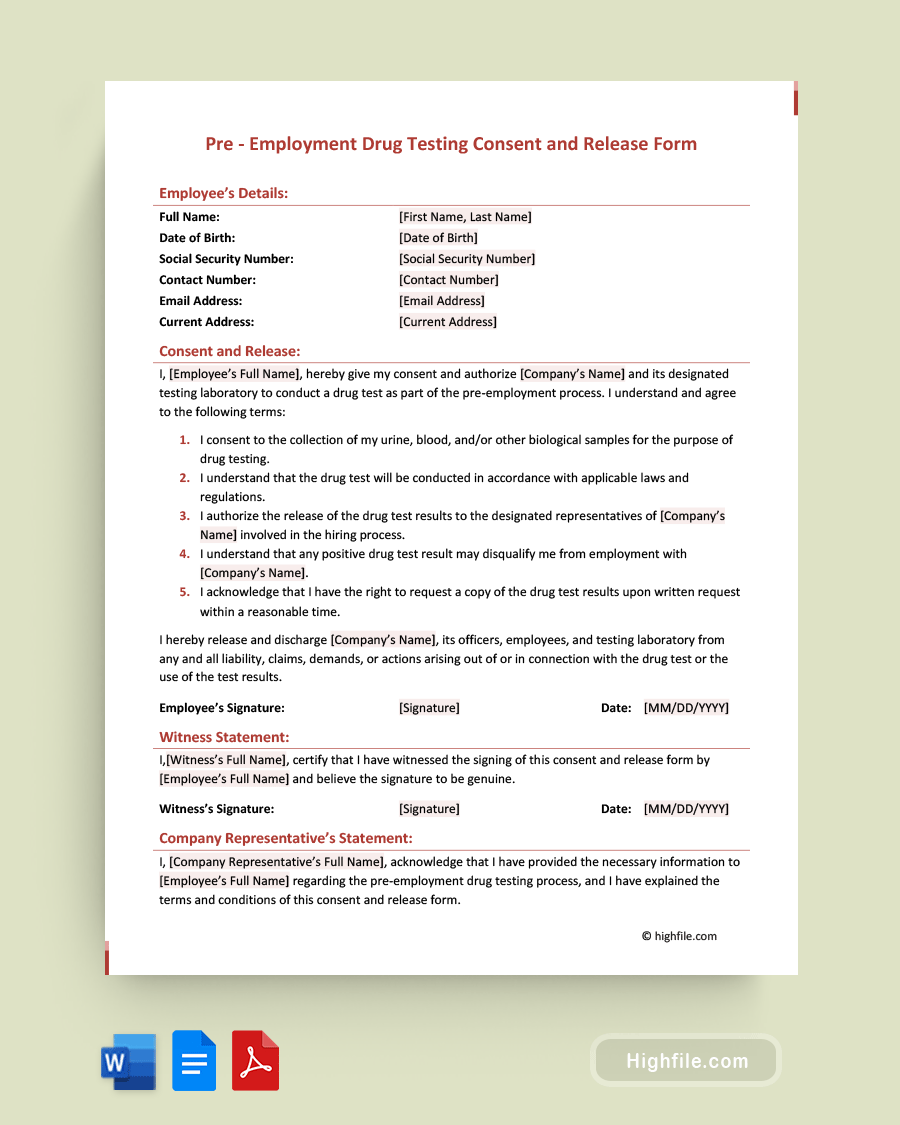
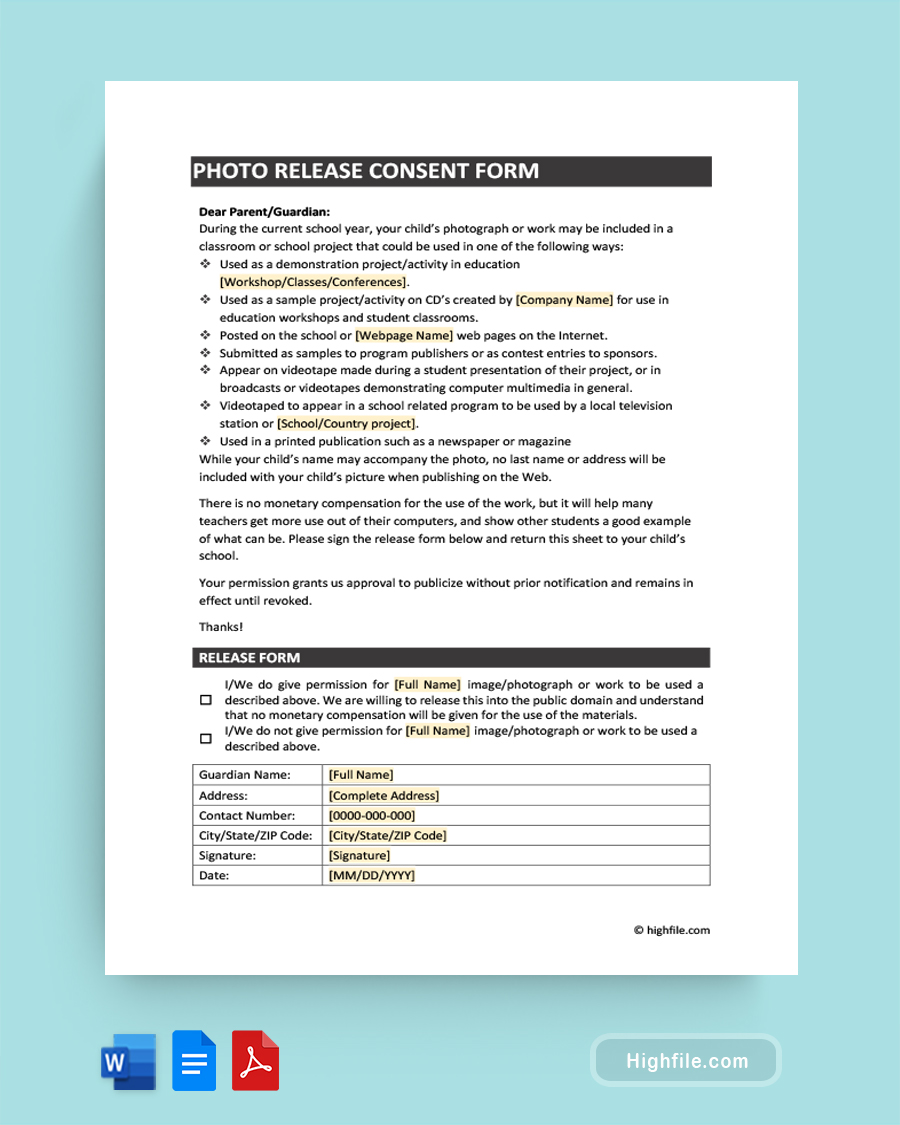
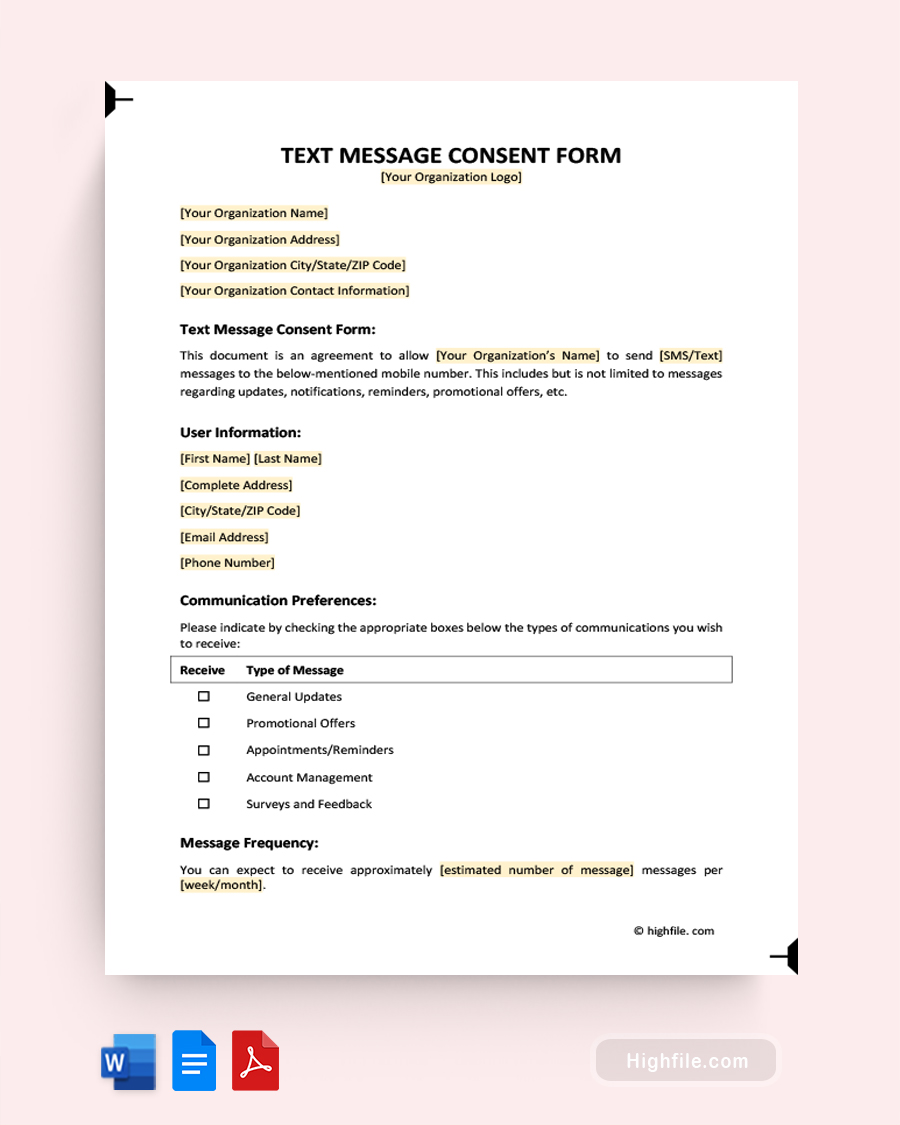
Patients must sign several additional forms and documents in addition to the IUD Consent Form template. These include an informed consent form outlining the risks and benefits of anesthesia, any agreements or paperwork required by the physician, a financial arrangement for payment of services, and a release of medical information form. Additionally, depending on the state, there may be a requirement for a patient to sign a separate document regarding their understanding of the contraceptive method being used. These forms can be created using a template.
The IUD Consent Form should be reviewed with the patient in person to ensure they understand the risks associated with the procedure. To ensure that the patient has a complete understanding of the risks, they must be given the opportunity to ask questions and receive answers from their healthcare provider. It is also beneficial for the patient to have the form in front of them during the discussion so they can refer to it if needed.
Final Thoughts
An IUD (intrauterine device) consent form is a document that a patient must sign before the placement of an IUD. This form outlines the risks and benefits of the procedure, as well as the patient’s rights and responsibilities. By signing the form, the patient agrees to the process and acknowledges that they understand its risks and benefits. The consent form also serves as a record of the patient’s informed consent for the procedure. Using a professionally created template helps reduce human error, save time, and provide an easy-to-use outline to ensure all the relevant and legally required information is included.