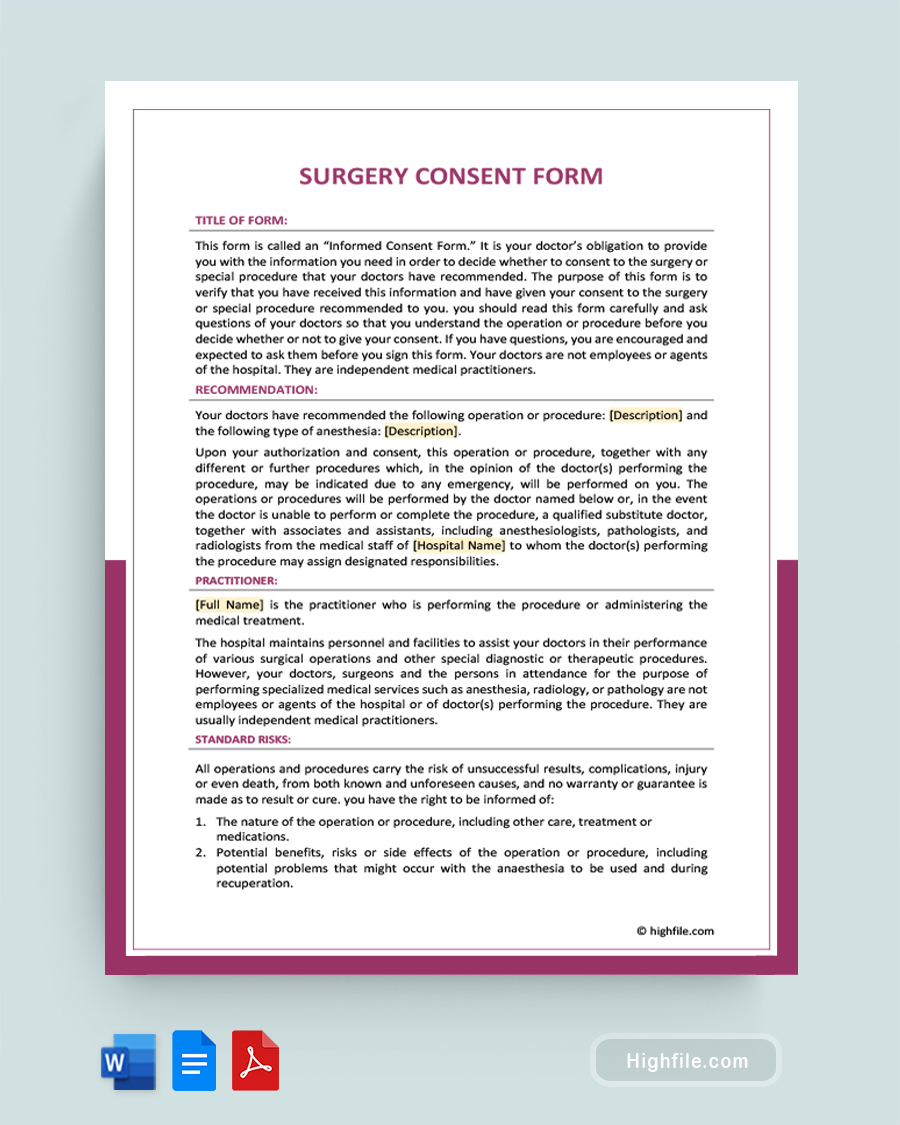
A surgery consent form is a critical part of the surgical documentation process. It is the form all patients are expected to sign before going into surgery. This is a legally binding contract that helps protect surgeons and respects patient rights to bodily autonomy. The patient signs this document to confirm that they have discussed the procedure with their doctor, understand it fully, and give consent to undergo the operation. A well-drafted consent form should outline the potential risks and benefits of the procedure, recommendations, conditions, alternatives, and other vital information. Since these forms often take several pages, we strongly recommend using our professional template to create these vital documents. Doing so helps save time and ensures that the surgeon and patient have communicated properly about the surgery.
What Is a Surgery Consent Form?
A surgery consent form is a legally binding document that shows a patient who is about to undergo surgery understands and consents to the procedure. It offers information about various aspects of their specific surgery and topics like anesthesia and blood transfusions, which are common, and ensures an open and honest dialogue between the medical practitioner and patient. Additionally, it helps protect surgeons and medical facilities from liability and legal action, which is especially important since it’s impossible to guarantee the outcome.
Why is a Surgery Consent Form Important?
Surgery consent forms are complex documents that cover numerous aspects of this vital medical procedure. We’ve created a list to help you understand why these forms are necessary and beneficial. Beyond merely being a required part of the documentation process, a lot goes into a basic surgery consent form.
- The consent form shows that a patient gave informed consent to undergo the procedure.
- It protects doctors, other medical professionals, and facilities from liability and litigation. Without these forms, doctors and facilities may be subject to malpractice, rebukes, or in extreme cases, loss of licensing and worse.
- It explains who recommended the process and why
- These forms contain information on alternatives
- They cover the risks and benefits
- Surgical consent forms tell the patient that the outcome is not guaranteed.
- These documents also inform patients about the risks of blood transfusions and anesthesia.
- They cover the side effects and expectations of success
- Surgery consent forms also have the doctor sign to indicate that they have thoroughly explained and discussed the proposed procedure with their patient
Essential Elements of a Surgery Consent Form
The essential elements of a surgery consent form are much more extensive than most traditional consent forms, primarily because surgery is complicated. These are often multi-page documents. Below we’ve created an outline to help you understand what should be included on this form and where it belongs.
- Logo or Facility Name
- A title in large bold print that says Surgery Consent Form or Informed Consent for Surgery
- Title of Form or About Section- This section explains that doctors are required to provide information and answers. It tells the reader to ask questions, read thoroughly, and understand what they are agreeing to before signing.
- Surgical Recommendation- Here, the form should have space for the doctor’s recommendation for surgery and anesthesia, along with a note that says who will be authorized to perform the surgery and any subsequent necessary surgeries or procedures.
- Practitioner Information- The practitioner information should show who the lead surgeon is and tell the patient that other doctors and medical staff may assist.
- Risks and Side Effects- It’s essential to inform the patient of the common risks and side effects.
- Anesthesia Information- Include a separate section on anesthesia so they understand any necessary information, such as potential risks and complications and any conditions they have that could cause complications.
- Blood Transfusion Information- Though not all patients need a blood transfusion, this section should be present in case a need arises. It should detail all the relevant information about risks, benefits, etc.
- Blood Transfusion Special Instructions- This is a space for notes, such as direct donation or pre-donation.
- Consent to Blood Transfusion Patient or Representative Signature, Date, and Time Lines- Have the patient sign their consent with the date and time of signature.
- Organ and Tissue Disposition Consent Statement- Typically, this leaves the disposition of anything removed from the body to the doctor or facility’s discretion. However, in some cases, it may be appropriate or necessary to honor the patient’s wishes, such as allowing them to bury a limb that has been removed.
- Organ and Tissue Disposition Patient or Representative Signature, Date and Time Lines- Have the patient sign their consent for this specific process.
- Conditions- If there are any additional conditions for the specific surgery, you should put them on the form.
- Statements of Assent- The statements of assent show that your patient has read and understood everything, spoken to their doctor, had any questions answered, and consented to the surgery.
- Patient or Representative Signature, Date, and Time Lines- Have the patient sign their overall consent. If the person signing was not the patient, they must put their name and relationship to the patient on a separate line. This primarily applies to powers of attorney and spouses for incapacitated adults and parents of minors.
- Interpreter or Reader Statement- If the patient needed an interpreter or someone to read for them, please include a statement showing that the person did everything in their power to convey the message precisely and completely.
- Interpreter or Reader Signature, Date, and Time Lines- The interpreter or reader signs, dates, and puts down the time here.
- Physician Certification- The physicians’ certification says that they have discussed all the relevant aspects of the surgery, provided reading materials if applicable, answered questions, and otherwise did their part to create an opportunity for informed consent.
- Physician Signature, Date, and Time Lines- Sign, date, and note down the time here.
Tips on How To Write a Surgery Consent Form Using a Template
Using a template to create your custom surgery consent form is quick and simple. Start by downloading the template. You can open it using MS Word, Adobe, Open Office, or most other writing programs. Next, you’ll fill in any blank sections. For example, you may need to import your logo and place it at the top of the page, fill in the recommendations, and include any additional information under the conditions section. You can also add any new or case-specific sections to your template as they become relevant.
You can leave space for blank lines to handwrite the individualized sections for patients and doctors instead if you plan to print off numerous copies to keep on hand. This works best for large facilities. Typing the details into each form is often a more sensible solution for smaller, private practices and medical businesses that see relatively few patients. Don’t forget to keep a blank copy of the template on hand so you can do the same for each patient.
FAQs
Surgery consent forms are complex documents with numerous requirements. In this section, we’ve answered some of the most frequently asked questions about surgery consent forms. You’ll learn more about who can sign, the legal implications of signing consent, and more.
Before any surgery, it is essential to obtain informed consent from the patient. This is because of the serious nature of the procedure and its potential risks. Even for low-risk procedures, this form is more than a mere formality. It is crucial. Informed consent requires that a patient be fully aware of all the risks and benefits of a particular surgery before agreeing to it. It also requires that they understand what will happen during and after the procedure and any alternatives available to them. By obtaining informed consent, surgeons can ensure that their patients make informed decisions about their health care.
The legal implications of signing a surgery consent form include understanding that this document is a legally binding agreement between the patient and the medical team that outlines the risks and benefits of the procedure. It also serves as a record of informed consent, which means that both parties have agreed to proceed with the surgery. Signing this document is an acknowledgment that all parties involved are aware of their rights and responsibilities before proceeding. It is also essential to protect patients and medical professionals from potential legal issues if something goes wrong during or after the surgery.
When a patient is unconscious and unable to sign a surgery consent form, it is important to know who can legally sign it on their behalf. Generally, the patient’s spouse has the legal right to sign the document. If no spouse is available, then a power of attorney, the parent or other close family members, such as an adult child or sibling, may sign. For minors, only a parent or legal guardian is authorized to sign the form.
All parties involved must know their rights and responsibilities, including respecting the patient’s wishes when signing such forms. However, the laws and requirements vary and are subject to change, so physicians and medical staff need to maintain a current understanding of what the law says about this in your area. If you are uncertain, consult an attorney.
The short answer is no. Performing any medical procedure without informed consent is a criminal act. However, in some cases, when the patient has no one to sign, no medical power of attorney listed, and they are utterly incapable of consent because they are unconscious or incapacitated, a life-saving surgery may be legally allowed. The implications and consequences of such an action can be severe. It is of the utmost importance to make sure you fully understand the possible outcome of performing such a procedure beforehand.
The patient’s treating physician is responsible for obtaining consent for a surgical procedure. In most cases, the person who submitted the referral, nurses, and other medical staff are not charged with handling this aspect of patient care. However, you should still ensure that the form is present and has been signed by all the appropriate parties before scheduling surgery.
Final Thoughts
Surgery is a serious medical procedure that carries certain risks. To make sure that patients understand the potential risks and complications associated with surgery, it is legally required for them to sign a surgery consent form. This document should clearly explain the risks, benefits, and purpose, but with no guarantees, either implicit or explicit, regarding the outcome of the surgery. It should also include a separate section on anesthesia and blood transfusions, as these are standard procedures in many surgeries. By signing this form, patients can be assured that their surgeon has provided them with all the necessary information about their surgery and any potential risks. Meanwhile, the surgeon and medical facility are protected against liability and legal action. Using a professionally designed template to create your surgery consent forms helps ensure you have all the appropriate information on the page and offers a framework to make the process quick and easy so you can get back to helping people.